Artificial intelligence in healthcare refers to computer systems that can analyze medical data and assist with patient care decisions traditionally made by humans.
Healthcare organizations worldwide have deployed AI systems across multiple medical specialties. The global healthcare AI market reached $11 billion in 2021 and projects to grow to $187 billion by 2030, according to industry research. The Food and Drug Administration has approved over 1,000 AI-containing medical devices through established regulatory pathways.

Source: Grand View Research
What Is AI in Healthcare
AI in healthcare means using computer programs that can learn patterns from medical information to help doctors and nurses take better care of patients. These systems work like very smart assistants that can spot things humans might miss and suggest helpful ideas for treatment.
Healthcare AI systems look at huge amounts of medical information — patient records, test results, X-rays, and treatment histories. They find patterns that people can’t see and give doctors useful insights. For example, IBM Watson Health reads medical research and patient data to help healthcare providers make treatment recommendations.
These AI tools handle everything from simple tasks like booking appointments to complex jobs like finding cancer in medical scans. Google’s DeepMind Health has built systems that can spot eye diseases from retinal photos just as well as specialist doctors. The technology has grown so much that the healthcare AI market jumped from $11 billion in 2021 to a projected $187 billion by 2030.
The way it works is pretty straightforward. Computer programs learn from thousands or millions of medical cases, just like medical students study many patient examples. Once trained, these systems can recognize similar patterns in new patients and give recommendations to healthcare providers.
Machine Learning in Medicine
Machine learning helps computers get better at medical tasks by studying lots of patient information. These algorithms learn the same way people do — by looking at many examples and finding patterns that help predict what might happen next.

Source: ResearchGate
Key ways machine learning helps in medicine include:
- Pattern recognition in medical imaging — Finding cancer cells in mammograms, spotting broken bones in X-rays, and detecting problems in MRI scans
- Lab result analysis — Flagging unusual blood test values that might show disease or dangerous drug combinations
- Treatment response prediction — Looking at how similar patients responded to treatments to guess likely outcomes
- Risk assessment — Checking patient factors to calculate chances of developing specific health problems
- Drug discovery — Finding potential new medications by analyzing how molecules work in the body
Medical imaging shows some of the biggest successes for machine learning in healthcare. Deep learning systems can find breast cancer in mammograms more accurately than human doctors in some studies. These systems analyze tiny details and subtle changes that human eyes might miss.
Lab data analysis lets machine learning systems spot unusual combinations of test results that might point to rare diseases or medication side effects. The algorithms can look at hundreds of lab values at once and compare them against patterns from millions of previous patients.
Natural Language Processing Applications
Natural language processing (NLP) helps computers read and understand medical notes, patient records, and other healthcare documents written in everyday language. NLP systems turn unorganized text into useful data that can help with patient care decisions.

Source: Maruti Techlabs
Healthcare NLP applications include:
- Clinical note analysis — Pulling out important medical concepts, symptoms, and diagnoses from doctors’ notes and nursing assessments
- Medical coding automation — Assigning correct billing and diagnostic codes to patient visits
- Drug monitoring — Finding medication mentions in clinical text and checking for dangerous interactions or allergies
- Quality measurement — Getting data needed for healthcare quality reports and compliance
- Research data extraction — Processing large amounts of medical literature to find relevant studies and findings
IBM’s Policy Insights with Watson shows advanced NLP by analyzing complex case files to highlight important information for healthcare workers. The system reads unstructured text to identify warning signs and protective factors, helping caseworkers handle multiple patient cases more efficiently.
NLP helps healthcare documentation by cutting down the time doctors spend on paperwork while making medical records more accurate. Systems can automatically fill out forms, suggest relevant medical codes, and make sure documentation meets regulatory requirements. For healthcare organizations looking to implement sophisticated NLP solutions, AI chatbot development services can provide custom tools for patient interaction and administrative tasks.
Predictive Analytics for Health
Predictive analytics uses AI to look at patient data and predict potential health problems, disease risks, and treatment responses before they happen. These systems examine patterns in medical history, current health status, demographics, and lifestyle factors to create probability assessments for different health scenarios.
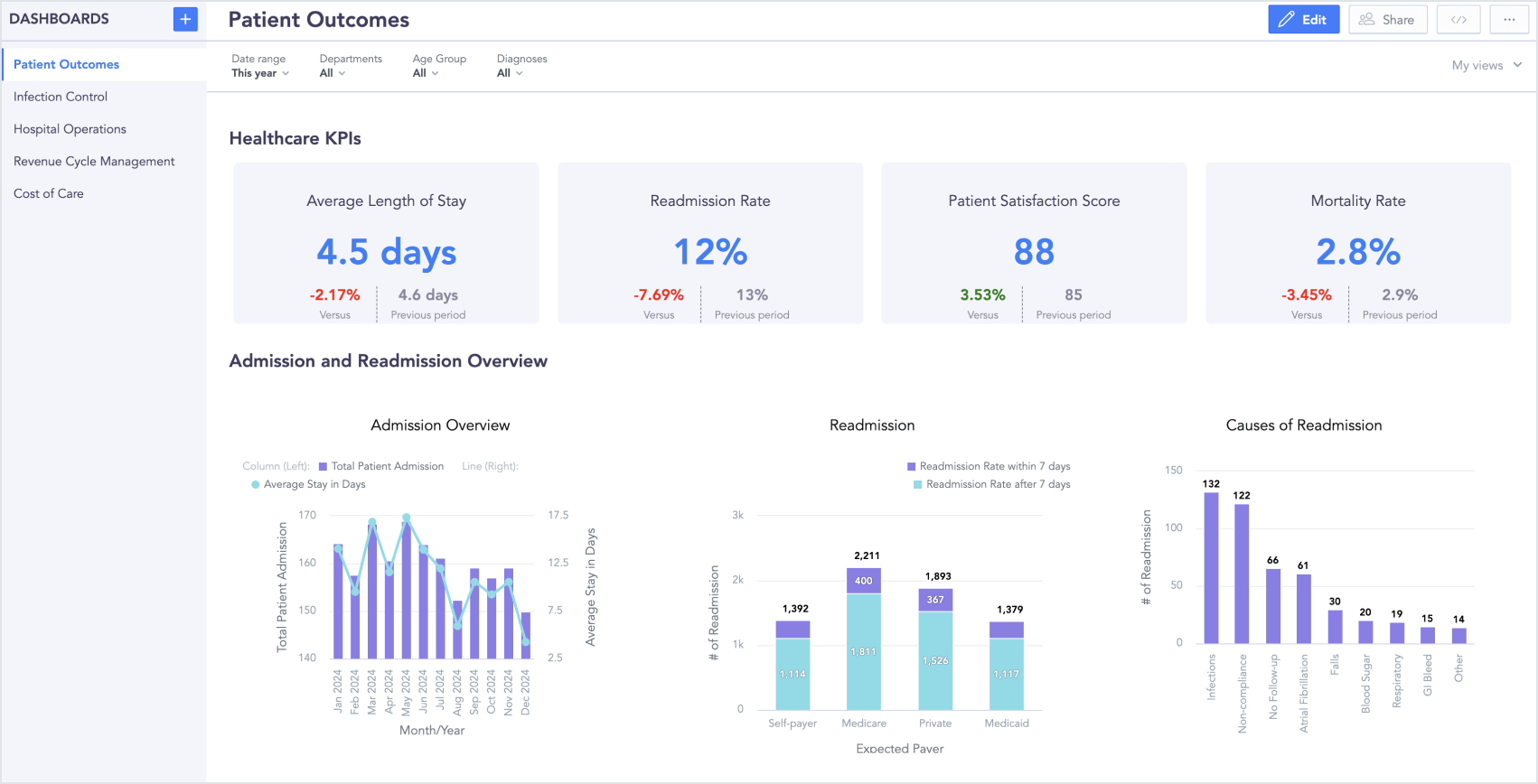
Source: GoodData
Healthcare organizations use predictive analytics to find patients at risk for hospital readmission, medication problems, or disease progression. For example, algorithms can analyze heart failure patients’ vital signs, lab results, and symptoms to predict which patients will likely need emergency care within the next 30 days.
Real examples of predictive healthcare applications include:
- Sepsis prediction — Monitoring patient vital signs and lab values to spot early warning signs of life-threatening infections
- Fall risk assessment — Analyzing patient mobility, medications, and medical history to predict likelihood of falls in hospitals
- Medication adherence forecasting — Predicting which patients will likely stop taking prescribed medications
- Disease progression modeling — Forecasting how chronic conditions like diabetes or kidney disease might advance over time
- Emergency department volume prediction — Helping hospitals prepare for patient surges by analyzing historical patterns and community health data
Preventive care benefits a lot from predictive analytics because early identification of health risks lets healthcare providers step in before conditions become serious. Patients identified as high-risk for developing diabetes can get lifestyle counseling and monitoring that may prevent or delay disease onset. Organizations implementing these analytics capabilities often benefit from generative AI development services to create custom predictive models tailored to their specific patient populations.
Current Applications of AI in Healthcare
AI has moved from experimental technology to essential healthcare infrastructure. Healthcare organizations worldwide use AI systems to improve patient care, cut costs, and boost efficiency across clinical and administrative functions.
Major technology companies have built comprehensive healthcare AI platforms that support different medical applications. IBM Watson Health processes huge medical datasets using cognitive computing, while Google’s DeepMind Health achieves diagnostic accuracy comparable to human experts in specialized fields like eye care.
Current AI applications span multiple areas including diagnostic imaging, drug discovery, clinical decision support, and operational management. The FDA has approved over 1,000 AI-containing medical devices, with 712 specifically in radiology applications.
Administrative Automation
AI systems make healthcare administration smoother by automating routine tasks that traditionally need lots of human work. Healthcare organizations report big time and cost savings through AI-powered administrative processes that work continuously with minimal human oversight.
Key administrative automation applications include appointment scheduling, insurance verification, claims processing, billing and coding, resource allocation, supply chain management, and patient registration. AI systems analyze provider availability, patient preferences, and clinical urgency to optimize scheduling while reducing wait times.
Healthcare organizations implementing these automation systems report processing time reductions of up to 70 percent for routine administrative tasks. Cost savings come through reduced staffing needs for repetitive processes while letting administrative staff focus on complex cases requiring human judgment.
For healthcare facilities looking to implement comprehensive administrative AI solutions, AI consulting for small businesses can provide customized automation strategies that fit specific organizational needs and budgets.
Clinical Documentation
AI-powered clinical documentation systems change how healthcare providers create, manage, and access medical records. These systems reduce physician administrative burden while improving documentation quality and consistency across healthcare organizations.
Automated transcription services convert doctor-patient conversations into structured clinical notes using natural language processing. Ambient listening technology captures clinical encounters without requiring physicians to interact directly with documentation systems during patient visits.
Medical coding assistance represents another significant application where AI systems analyze clinical notes and automatically suggest appropriate diagnostic and procedure codes. These systems reduce coding errors while ensuring compliance with billing requirements and quality reporting standards.
Real-time documentation assistance provides immediate feedback during clinical encounters, alerting physicians to potential documentation gaps or inconsistencies that could impact patient care or billing accuracy. Template optimization features customize documentation workflows based on physician preferences and specialty requirements.
Patient Monitoring Systems
AI-enhanced patient monitoring extends healthcare capabilities beyond traditional clinical settings through continuous data collection and analysis. Remote monitoring devices equipped with machine learning algorithms detect subtle changes in patient conditions that might indicate health problems before symptoms become apparent.
Wearable devices monitor vital signs, activity levels, sleep patterns, and other body measurements continuously. AI algorithms analyze this data to identify patterns indicating potential health issues such as irregular heart rhythms, blood sugar changes, or early signs of infection.
Hospital-based monitoring systems use AI to analyze patient data from multiple sources including electronic health records, laboratory results, vital sign monitors, and medication administration records. Early warning systems alert healthcare providers when patient conditions suggest increased risk for complications such as sepsis, cardiac events, or breathing problems.
Post-discharge monitoring applications track patient recovery and medication adherence following hospital stays or surgical procedures. AI systems analyze patient-reported symptoms, activity data, and body measurements to identify patients needing additional support or clinical intervention.
Telemedicine Enhancement
AI technologies improve telemedicine capabilities by providing sophisticated diagnostic assistance and clinical decision support during virtual consultations. These systems expand healthcare access to underserved populations while maintaining clinical quality standards comparable to in-person visits.
Virtual triage systems analyze patient symptoms and medical history to determine appropriate care levels and urgency. AI algorithms can assess symptom severity, recommend emergency care when necessary, or direct patients to appropriate healthcare providers based on their specific needs.
Diagnostic assistance during telemedicine encounters includes AI-powered analysis of images patients capture using smartphone cameras or specialized devices. Skin care applications can analyze skin lesions to identify potential cancers or inflammatory conditions. Eye care tools assess eye conditions through smartphone-based photography.
Language translation services powered by AI help healthcare providers communicate effectively with patients who speak different languages. Real-time translation capabilities include medical terminology and cultural considerations specific to healthcare contexts.
Benefits of AI in Healthcare
AI transforms healthcare by improving diagnostic accuracy, reducing costs, enhancing patient outcomes, and increasing operational efficiency. AI systems analyze vast amounts of medical data faster and more consistently than traditional methods, helping healthcare providers make better-informed decisions and deliver more effective care.
AI reduces human error through consistent analysis of medical data. Machine learning algorithms process information without fatigue or subjective interpretation, maintaining the same level of accuracy regardless of time of day or workload.
Healthcare organizations benefit from data-driven decision making through AI’s ability to analyze patient records, treatment outcomes, and clinical research simultaneously. These systems identify optimal treatment pathways by comparing current cases with thousands of similar historical cases.
Improved Diagnostic Accuracy
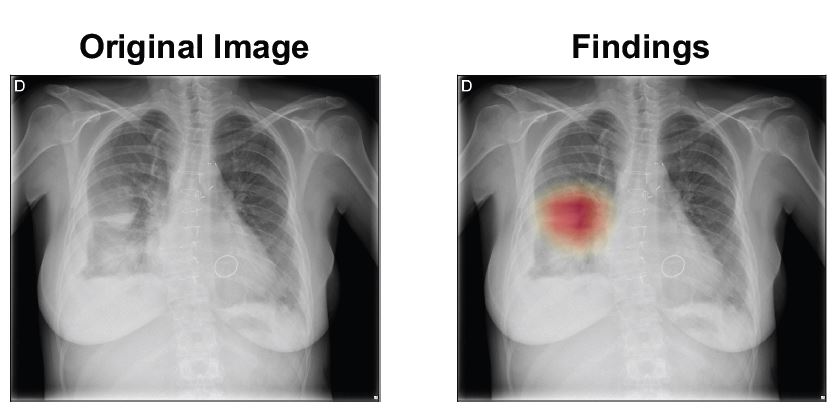
AI systems enhance diagnostic accuracy by detecting subtle patterns in medical images and patient data that human observers might miss. Radiology departments benefit significantly from AI assistance, with machine learning algorithms identifying early-stage cancers, fractures, and other abnormalities in X-rays, CT scans, and MRIs.
In mammography screening, AI systems detect breast cancer signs that radiologists occasionally overlook during routine examinations. These algorithms analyze tissue density patterns, calcium deposits, and structural changes with precision that exceeds human visual capabilities in certain scenarios.
Pathology laboratories use AI to analyze tissue samples and blood work with greater consistency than manual examination alone. Machine learning algorithms identify cellular abnormalities, measure tissue characteristics, and classify disease states based on microscopic features.
AI diagnostic tools process chest X-rays to identify pneumonia, tuberculosis, and other breathing conditions faster than traditional interpretation methods. Emergency departments benefit from rapid AI screening that prioritizes urgent cases and identifies patients requiring immediate attention.
Reduced Healthcare Costs
AI reduces healthcare costs through improved efficiency, reduced redundant testing, and prevention of medical errors. Healthcare organizations save money by automating routine tasks, optimizing resource allocation, and reducing the length of patient stays through faster diagnosis and treatment.
Administrative cost savings result from AI automation of appointment scheduling, insurance verification, and medical coding. Natural language processing systems extract relevant information from clinical notes and automatically generate appropriate billing codes, reducing manual data entry requirements.
AI prevents costly medical errors by identifying potential drug interactions, flagging unusual dosages, and alerting providers to patient allergies or contraindications. These safety systems reduce adverse events that lead to extended hospital stays, additional treatments, and legal claims.
Predictive analytics help healthcare organizations optimize staffing levels, equipment use, and supply chain management. AI systems forecast patient volume, identify seasonal trends, and predict resource needs, allowing hospitals to operate more efficiently without compromising care quality.
Enhanced Patient Outcomes
AI improves patient outcomes by enabling faster treatment initiation, personalizing care plans, and predicting health risks before they become critical. Patients receive more targeted therapies based on their individual characteristics, medical history, and genetic profiles.
Emergency departments use AI triage systems to prioritize patients based on symptom severity and likelihood of serious conditions. These systems ensure that critical cases receive immediate attention while efficiently managing patient flow during busy periods.
Personalized treatment plans benefit from AI analysis of patient genetics, lifestyle factors, and treatment response patterns. Machine learning algorithms identify which medications and dosages work best for individual patients based on their biological characteristics and medical history.
Chronic disease management improves through AI monitoring of patient data from wearable devices, home monitoring equipment, and regular check-ins. These systems detect early signs of disease progression and alert healthcare providers when interventions are needed.
Increased Operational Efficiency
AI streamlines healthcare operations by automating routine tasks, optimizing workflows, and reducing administrative burden on clinical staff. Healthcare professionals spend more time on direct patient care when AI handles documentation, scheduling, and data analysis tasks.
Electronic health record systems enhanced with AI automatically populate clinical notes, extract relevant information from previous visits, and suggest appropriate documentation templates. These features reduce the time physicians spend on administrative tasks and improve documentation completeness and accuracy.
Radiology departments benefit from AI assistance in image analysis workflow management. Machine learning algorithms prioritize urgent scans, automatically measure anatomical structures, and generate preliminary reports for radiologist review.
Hospital bed management systems use AI to predict patient discharge times, identify bed availability, and optimize patient placement throughout the facility. These systems reduce wait times for admissions and improve resource use during peak demand periods.
AI in Medical Diagnosis and Imaging
Medical diagnosis represents one of the most impactful applications of AI in healthcare today. AI systems excel at analyzing patterns in medical data that human eyes might miss or take significantly longer to identify. These technologies work alongside healthcare professionals to enhance diagnostic accuracy and speed.
The foundation of AI-powered medical diagnosis lies in machine learning algorithms trained on vast datasets of medical images, laboratory results, and patient records. These systems learn to recognize subtle patterns, abnormalities, and connections that indicate specific diseases or conditions.
Radiology and Medical Imaging
Radiology has become the leading specialty for AI implementation in healthcare, with systems that can analyze medical images faster and often more accurately than traditional methods. AI algorithms process multiple types of imaging studies, identifying potential abnormalities and helping radiologists make more precise diagnoses.
Source: European Society of Radiology
Common imaging types enhanced by AI include X-rays for detecting fractures, pneumonia, tuberculosis, and bone abnormalities; CT scans for identifying tumors, blood clots, internal bleeding, and stroke indicators; MRI scans for detecting brain tumors, multiple sclerosis lesions, torn ligaments, and joint problems; mammograms for identifying suspicious masses, calcium deposits, and tissue patterns; and ultrasounds for identifying fetal abnormalities during pregnancy and detecting organ problems.
AI systems have demonstrated the ability to reduce chest X-ray interpretation times from over 11 days to under 3 days while improving diagnostic accuracy. In breast cancer screening, AI-powered analysis equals or surpasses human radiologist performance in detecting cancers while significantly reducing false-positive results.
Pathology Analysis
Pathology represents another medical specialty where AI provides substantial diagnostic support through automated analysis of tissue samples, blood tests, and cellular patterns. Digital pathology systems use high-resolution microscopy images that AI algorithms can examine at the cellular level.
AI pathology systems analyze tissue biopsies by examining cell shape, tissue structure, and staining patterns. These algorithms can count cells, measure tissue features, and identify abnormal cellular structures that pathologists use to diagnose diseases.
Laboratory analysis benefits from AI systems that interpret blood tests, urine samples, and other laboratory results. Algorithms can identify abnormal values, suggest additional tests, and connect findings with patient symptoms and medical history.
The collaboration between AI and pathologists improves diagnostic consistency and reduces the time required for complex analyses. AI systems can process routine cases quickly, allowing pathologists to focus their expertise on challenging diagnoses that require human interpretation and clinical context.
Early Disease Detection
AI excels at identifying subtle patterns in medical data that may indicate disease development before obvious symptoms appear. Predictive algorithms analyze patient demographics, medical history, genetic factors, and current health status to calculate risk scores for various conditions.
Early detection capabilities span multiple disease categories. AI systems can identify patients at high risk for heart disease by analyzing electrocardiogram patterns, blood pressure trends, and laboratory values. Cancer screening benefits from AI algorithms that detect microscopic changes in imaging studies that come before visible tumor development.
Eye damage from diabetes receives early intervention through AI analysis of retinal photographs that identify eye damage before vision problems occur. Kidney disease progression can be predicted through AI evaluation of laboratory trends and patient risk factors, enabling preventive treatments that preserve organ function.
Preventive screening programs use AI to identify individuals who would benefit most from specific diagnostic tests based on their risk profiles. These systems optimize healthcare resources by focusing screening efforts on patients most likely to have undiagnosed conditions.
Computer-Aided Diagnosis
Computer-aided diagnosis systems represent a mature form of AI implementation that supports rather than replaces physician decision-making. These tools provide second opinions, highlight potential findings, and offer diagnostic suggestions based on medical evidence and patient data.
AI diagnostic support systems connect with electronic health records to access comprehensive patient information including previous test results, medications, and medical history. Algorithms consider multiple data sources at once to provide diagnostic recommendations that account for individual patient characteristics and clinical context.
The collaborative relationship between AI and healthcare providers maintains physician authority over diagnostic decisions while providing technological assistance that enhances accuracy and efficiency. AI systems flag potential diagnoses for physician review, suggest additional tests that might be helpful, and provide relevant medical literature citations.
Modern AI diagnostic tools operate transparently, showing healthcare providers how algorithms reach their conclusions and what factors influence their recommendations. This explainable AI approach allows physicians to evaluate AI suggestions critically and incorporate them appropriately into their clinical reasoning processes.
AI in Drug Discovery and Development
The pharmaceutical industry faces a costly challenge: developing new medications typically takes 10-15 years and costs over $2.6 billion per approved drug. AI is transforming how researchers discover, test, and bring new treatments to market.

Source: Research Communities by Springer Nature
Machine learning algorithms process genetic data, protein structures, and disease pathways to identify promising therapeutic targets faster than conventional methods. AI also evaluates how different compounds might interact with specific biological targets, helping researchers design more effective medications with fewer side effects.
Target Identification
AI systems excel at finding new drug targets by analyzing massive biological databases that would take human researchers years to process manually. These algorithms examine genetic information, protein interaction networks, and cellular pathways to identify specific molecules or biological processes that contribute to disease.
Traditional target identification involves researchers manually reviewing scientific literature and conducting laboratory experiments to understand how diseases develop at the molecular level. AI accelerates this process by simultaneously analyzing thousands of research papers, genetic studies, and molecular databases to spot patterns.
Machine learning models can predict which proteins or cellular processes play key roles in specific diseases by examining how genetic variations affect patient outcomes. For example, an AI system might analyze genetic data from cancer patients to identify proteins that appear consistently altered in tumor cells but remain normal in healthy tissue.
Organizations implementing AI-powered drug discovery platforms often benefit from generative AI development services to create custom algorithms that can identify novel therapeutic targets specific to their research focus.
Clinical Trial Optimization
AI transforms clinical trials by improving how researchers select participants, design studies, and predict outcomes. Machine learning algorithms analyze patient medical records, genetic profiles, and health histories to identify individuals most likely to benefit from experimental treatments.
Traditional patient recruitment for clinical trials often takes months or years, with researchers manually reviewing thousands of medical records to find qualified participants. AI systems can screen electronic health records in hours, identifying patients who meet specific criteria while flagging potential safety concerns or drug interactions.
Large language models demonstrate remarkable accuracy in patient screening, achieving 97.9 percent accuracy compared to 91.7 percent accuracy from human reviewers in heart failure studies. AI-based patient eligibility screening costs approximately $0.11 per patient using automated systems.
Trial design optimization represents another AI application where algorithms analyze historical trial data to recommend optimal study protocols, dosing schedules, and measurement points. AI systems can predict which trial designs are most likely to succeed based on similar previous studies.
Personalized Medicine
AI enables personalized medicine by analyzing individual genetic profiles, biomarkers, and treatment response patterns to recommend optimal therapies for specific patients. Machine learning algorithms process genetic data alongside clinical information to predict which medications will work best for individual patients.
Genetic variations affect how patients process medications, respond to treatments, and develop side effects. AI systems analyze these genetic differences alongside clinical data to identify patient subgroups that share similar biological characteristics and treatment responses.
Drug processing applications use AI to predict drug responses based on genetic markers that affect medication breakdown. For instance, AI algorithms can identify patients who process certain medications slowly, requiring lower doses to avoid toxicity, or patients who process drugs rapidly, needing higher doses for therapeutic effect.
Treatment outcome prediction represents an advanced application where AI analyzes patient data including genetics, medical history, and biomarkers to forecast how individuals will respond to specific therapies. These predictions help physicians choose optimal treatment strategies while avoiding medications likely to cause adverse reactions.
Regulatory Approval Acceleration
AI streamlines regulatory approval processes by automating documentation preparation, analyzing clinical trial data, and predicting regulatory outcomes. Machine learning systems can organize vast amounts of clinical trial data into standardized formats required for regulatory submissions.
The FDA has developed frameworks specifically for AI-enabled drug development, recognizing both the technology’s potential and unique evaluation challenges. Predetermined Change Control Plans allow AI systems to evolve and improve over time while maintaining safety standards.
Documentation automation represents a significant efficiency gain where AI systems can generate regulatory submission documents by analyzing clinical trial results, safety data, and effectiveness measurements. Natural language processing algorithms can extract key findings from research papers and clinical reports.
Regulatory agencies increasingly use AI tools themselves to review submissions more efficiently. These systems can identify potential safety signals, analyze clinical trial designs for adequacy, and flag submissions requiring additional human review based on complexity or risk factors.
AI in Clinical Decision Support and Patient Care
AI transforms how healthcare providers make treatment decisions and deliver patient care. AI systems analyze vast amounts of medical data to provide evidence-based recommendations that support clinical judgment rather than replace it.
Clinical decision support systems powered by AI process patient demographics, medical history, laboratory results, and imaging studies to generate insights that inform treatment planning. Healthcare providers use these AI-generated recommendations alongside their clinical experience to make more informed decisions about patient care.

Source: ResearchGate
Treatment Recommendation Systems
AI treatment recommendation systems analyze patient-specific data to suggest optimal therapeutic approaches based on evidence from large medical databases and clinical research. These systems compare individual patient characteristics with outcomes from similar cases to identify treatments most likely to succeed.
Machine learning algorithms process genetic information, biomarkers, medical history, and current health status to generate personalized treatment recommendations. For example, AI systems can analyze cancer patient data to suggest chemotherapy regimens that have shown the highest success rates for patients with similar genetic profiles and disease characteristics.
Treatment recommendation systems continuously learn from new patient outcomes and medical research to refine their suggestions. When physicians document treatment results in electronic health records, AI systems incorporate this feedback to improve future recommendations.
These systems also alert providers to potential drug interactions, contraindications, and alternative treatment options that might not be immediately apparent during clinical encounters. Organizations implementing these sophisticated decision support tools often work with AI consulting services to customize recommendations based on their specific patient populations and clinical protocols.
Risk Assessment Tools
Predictive AI models analyze patient data to identify individuals at high risk for complications, hospital readmissions, and adverse events. These tools process electronic health record information, laboratory values, vital signs, and medication lists to generate risk scores.
Risk assessment algorithms can predict which patients will likely develop sepsis, experience cardiac events, or require intensive care unit admission. Early warning systems continuously monitor patient data and alert healthcare providers when risk scores exceed predetermined levels.
Readmission risk models help healthcare teams identify patients who need additional support during care transitions. These systems analyze factors such as previous hospitalizations, chronic conditions, social factors, and medication complexity to predict which patients will most likely return to the hospital within 30 days.
Adverse event prediction systems monitor patients for signs of medication reactions, falls, or other safety concerns. AI algorithms analyze patterns in vital signs, laboratory results, and clinical notes to identify early indicators of potential problems.
Patient Engagement Platforms
AI-powered patient engagement platforms provide 24/7 health support through chatbots, mobile applications, and virtual health assistants. These tools answer routine medical questions, provide health education, and help patients manage chronic conditions between clinical visits.
Health chatbots can handle appointment scheduling, medication reminders, and basic symptom assessment. When patients report concerning symptoms, these systems can recommend appropriate levels of care, from self-management strategies to urgent medical attention.
Educational platforms use AI to deliver personalized health information based on individual patient conditions and learning preferences. These systems adapt content complexity and presentation format to match patient health literacy levels.
Medication adherence platforms track patient compliance with prescribed treatments and provide personalized interventions to improve adherence rates. AI systems analyze patterns in medication taking behavior and identify optimal timing and methods for reminders. Healthcare organizations looking to implement comprehensive patient engagement solutions can benefit from AI chatbot development services to create custom platforms tailored to their patient populations.
Remote Monitoring Solutions
Remote monitoring systems use AI to analyze continuous patient data from wearable devices, home monitoring equipment, and patient-reported symptoms. These platforms track vital signs, activity levels, sleep patterns, and other health indicators.
Continuous glucose monitors for people with diabetes use AI algorithms to predict blood sugar trends and recommend insulin adjustments. These systems learn individual patient patterns and provide personalized alerts when glucose levels will likely become problematic.
Heart failure monitoring systems track daily weights, blood pressure, and activity levels to identify early signs of condition worsening. AI algorithms can detect subtle patterns that might not be apparent to patients or providers, such as gradual weight gain combined with decreased activity levels.
Chronic disease management platforms integrate data from multiple sources to provide comprehensive health tracking. Patients with conditions such as high blood pressure, chronic lung disease, or arthritis can use these systems to monitor symptoms, track medication effectiveness, and communicate with healthcare providers.
Challenges and Limitations of AI in Healthcare
While AI offers significant benefits for healthcare, implementing these systems creates substantial challenges that organizations must address. Healthcare AI faces obstacles in data quality, algorithmic bias, system integration, and regulatory compliance that can impact patient safety and treatment effectiveness.

Source: NannyML
The complexity of healthcare environments means AI systems must operate within existing workflows while meeting strict safety and privacy standards. These challenges require ongoing attention and resources to resolve, though industry leaders continue developing solutions to address current limitations.
Data Quality and Privacy Concerns
Healthcare AI systems depend entirely on the quality of data used to train and operate them, but medical records often contain incomplete information, coding errors, and inconsistent documentation practices. The National Institute of Standards and Technology emphasizes that poor data quality leads directly to unreliable AI outputs.
HIPAA compliance creates additional complexity when AI systems process protected health information. Healthcare organizations must ensure AI applications properly handle, store, and transmit patient data while meeting federal requirements for privacy protection and breach notification.
Patient confidentiality becomes more challenging when AI systems involve third-party vendors or cloud-based processing. Organizations establish Business Associate Agreements that clearly define data protection responsibilities, implement encryption for data transmission and storage, and maintain audit trails.
Healthcare institutions address these privacy concerns through comprehensive security frameworks that include access controls, regular security assessments, and staff training on data protection protocols. Many organizations also implement data de-identification techniques that remove personally identifiable information before AI processing. Organizations implementing robust AI data management systems can better address these privacy and quality challenges while maintaining compliance.
Algorithmic Bias Issues
Algorithmic bias occurs when AI systems produce unfair or discriminatory results for different patient populations, typically because training data reflects historical inequalities in healthcare delivery. Research demonstrates that AI systems can perpetuate existing healthcare disparities by prioritizing certain demographic groups over others.
Training data bias emerges when historical medical records contain unequal representation of different populations or reflect past discriminatory practices. For example, AI systems trained on data from predominantly white patient populations may perform poorly when analyzing cases from other ethnic groups.
Healthcare organizations work to address bias through careful data curation that ensures training datasets represent diverse patient populations. Developers implement bias detection algorithms that test AI system performance across different demographic groups and identify areas where the system produces unequal outcomes.
Ongoing bias mitigation efforts include regular auditing of AI system decisions, diverse development teams that bring different perspectives to AI design, and transparency requirements that allow healthcare providers to understand how AI systems reach their conclusions. These initiatives align with broader AI compliance frameworks that ensure responsible AI implementation.
Integration Complexities
Integrating AI systems with existing electronic health record platforms creates technical challenges that require significant infrastructure investments and workflow modifications. Healthcare organizations must ensure AI applications communicate effectively with current systems while minimizing disruption to clinical operations.
Interoperability standards like HL7 FHIR help AI systems access and exchange healthcare data, but implementation requires careful coordination between AI vendors, EHR providers, and healthcare IT teams. Many healthcare organizations discover that their current systems lack the technical capabilities needed to support advanced AI applications.
Healthcare providers must adapt their workflows to incorporate AI recommendations while maintaining clinical oversight and professional judgment. Staff training becomes essential as healthcare professionals learn to interpret AI outputs, understand system limitations, and integrate AI insights with their clinical expertise.
Ongoing efforts to improve integration include developing standardized AI interfaces that work across different EHR platforms, creating plug-and-play AI modules that require minimal technical configuration, and establishing best practices for AI workflow integration.
Regulatory Compliance Requirements
The FDA has approved over 1,000 AI-containing medical devices through established regulatory pathways, but the approval process requires extensive validation studies that demonstrate safety and effectiveness. Healthcare organizations must navigate complex regulatory requirements that vary depending on the specific AI application.
Safety standards for AI systems include requirements for performance monitoring, bias assessment, and transparency that allow healthcare providers and patients to understand how systems make decisions. The FDA requires predetermined change control plans for AI systems that learn and adapt over time.
Validation requirements involve demonstrating that AI systems perform accurately across diverse patient populations and clinical scenarios. Developers must provide evidence that their systems work reliably in real-world healthcare environments, not just controlled research settings.
Regulatory compliance extends beyond FDA requirements to include state licensing regulations for telemedicine applications, HIPAA privacy rules, and evolving standards for AI system documentation and monitoring. Healthcare organizations establish compliance frameworks that track regulatory changes and require robust AI governance structures to ensure ongoing compliance.
Regulatory Landscape for Healthcare AI
Healthcare AI operates within a complex regulatory environment that continues to evolve as AI technologies advance. Multiple agencies, standards organizations, and governing bodies work together to ensure AI systems meet safety and effectiveness requirements before deployment in clinical settings.
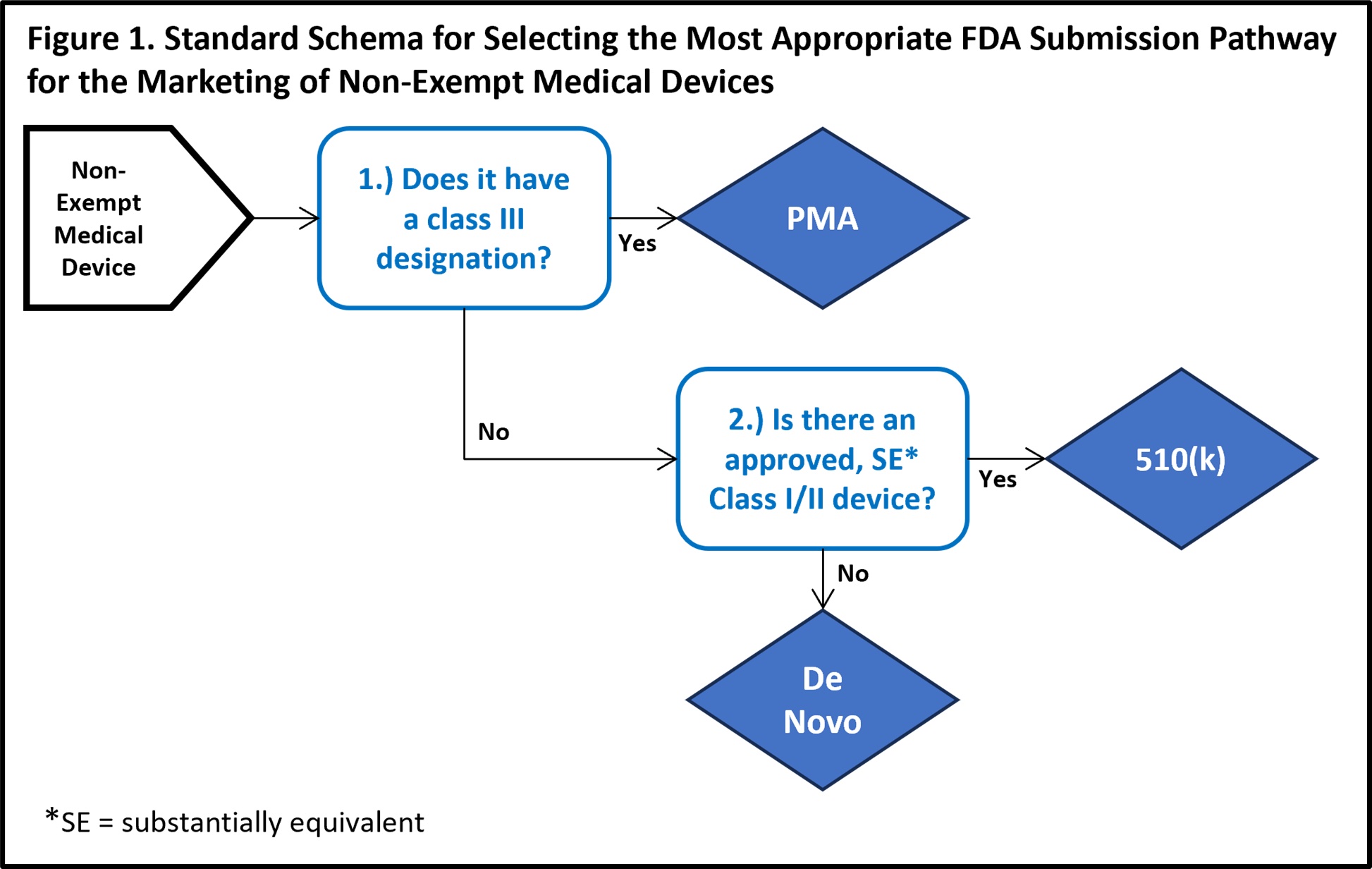
Source: MedTech Intelligence
The regulatory framework addresses unique challenges that AI systems present compared to traditional medical devices. Machine learning algorithms can change their behavior over time as they process new data, creating oversight challenges that didn’t exist with static medical equipment.
FDA Approval Processes
The Food and Drug Administration has approved over 1,000 AI-containing medical devices through established premarket pathways. The majority of these approvals concentrate in radiology applications, where AI systems analyze medical images to detect diseases and abnormalities.
The FDA categorizes AI tools under Clinical Decision Support Software (CDS) classification. Software that acquires, processes, or analyzes medical images, signals, or patterns typically requires regulatory review. Tools that provide recommendations to healthcare providers without specific outputs may be exempt from approval requirements.
The agency has developed Predetermined Change Control Plans to address AI systems that learn and adapt over time. These plans allow manufacturers to update AI models while maintaining safety standards without requiring separate marketing submissions for each modification.
The Digital Health Center of Excellence has modernized approval processes to handle hundreds of AI applications efficiently. The FDA provides a Digital Health Policy Navigator to help developers determine whether their AI applications require regulatory oversight based on functionality, clinical risk, and intended use.
HIPAA Compliance Considerations
AI systems processing protected health information must comply with Health Insurance Portability and Accountability Act requirements. Healthcare organizations implementing AI face complex privacy obligations when these systems access, analyze, or store patient data.
Privacy requirements extend beyond basic data protection to include specific safeguards for AI processing activities. Organizations must ensure AI systems appropriately handle patient information during training, inference, and storage phases.
Third-party AI vendors typically require Business Associate Agreements that clearly define responsibilities for data protection and regulatory compliance. These agreements specify how vendors will safeguard protected health information, respond to data breaches, and maintain audit trails for AI system activities.
Security measures for AI systems include encryption of data in transit and at rest, access controls that limit system users to authorized personnel, and monitoring systems that detect unauthorized access attempts. Healthcare organizations must implement breach notification procedures specific to AI systems. For comprehensive privacy protection, healthcare organizations often implement advanced privacy policy frameworks that address AI-specific data handling requirements.
International Standards
Global regulatory approaches to healthcare AI vary significantly across jurisdictions, though harmonization efforts seek to establish consistent evaluation standards. The European Union has implemented comprehensive AI regulation through the AI Act, which establishes risk-based oversight frameworks for AI applications in healthcare.
The EU AI Act categorizes healthcare AI systems based on risk levels, with high-risk applications requiring strict oversight and certain AI uses facing complete prohibitions. Medical devices incorporating AI must meet both AI-specific requirements and existing medical device regulations.
Canada has established the Directive on Automated Decision-Making for government AI services, requiring risk assessments and impact evaluations for AI systems used in public healthcare settings. The directive includes requirements for algorithmic impact assessments and public reporting of AI system performance.
Singapore has developed model AI governance frameworks that emphasize voluntary adoption of best practices while providing structured approaches to AI risk management. These frameworks include sector-specific guidance for healthcare AI applications and requirements for algorithmic auditing.
Ethics and Governance Frameworks
Responsible AI development in healthcare requires comprehensive governance frameworks that address algorithmic bias, transparency, and fairness throughout the AI lifecycle. These frameworks establish principles and processes for ethical AI design, deployment, and monitoring.
Transparency requirements emphasize explainable AI systems that provide clear rationales for their recommendations and decisions. Healthcare providers and patients need to understand how AI systems reach conclusions, particularly for applications involving diagnosis or treatment recommendations.
Accountability frameworks assign responsibility for AI system decisions across development teams, healthcare organizations, and clinical users. These frameworks specify who bears responsibility when AI systems make errors or produce biased outcomes that affect patient care.
Fairness principles require AI systems to perform equitably across diverse patient populations without discriminating based on race, gender, age, socioeconomic status, or other protected characteristics. Organizations must test AI systems for bias and implement mitigation strategies when different performance is detected. Healthcare organizations implementing comprehensive governance frameworks often benefit from specialized AI management standards that provide structured approaches to responsible AI implementation.
Future of AI in Healthcare
Healthcare stands at the beginning of a technological revolution that will reshape how medical professionals diagnose diseases, develop treatments, and deliver patient care over the next decade. AI technologies continue evolving rapidly, creating new possibilities for improving patient outcomes while addressing persistent challenges in healthcare accessibility and efficiency.

Source: Waymark | Digital
The trajectory of AI development in healthcare points toward increasingly sophisticated applications that integrate multiple technologies to create comprehensive healthcare solutions. These advances build upon current successes in diagnostic imaging and clinical decision support while expanding into areas that were previously impossible to automate.
Emerging Technologies
Quantum computing represents one of the most significant technological developments that will transform healthcare AI capabilities. Quantum computers process information using quantum mechanical principles, allowing them to solve complex problems exponentially faster than traditional computers.
Drug discovery applications of quantum computing could reduce the time required to develop new medications from decades to months. Quantum algorithms can simulate molecular interactions with unprecedented accuracy, enabling researchers to predict how potential drugs will behave in the human body before conducting expensive laboratory experiments.
Advanced robotics integrated with AI creates autonomous systems capable of performing complex medical procedures with precision that exceeds human capabilities. Surgical robots equipped with machine learning algorithms adapt to individual patient anatomy in real-time, making microscopic adjustments during operations to optimize outcomes.
Brain-computer interfaces represent an emerging frontier where AI systems interpret neural signals directly from the human brain. These interfaces allow paralyzed patients to control prosthetic limbs, computer cursors, and communication devices through thought alone.
Market Growth Projections
Healthcare AI adoption accelerates as organizations recognize the technology’s capacity to improve patient outcomes while reducing operational costs. Healthcare systems invest heavily in AI infrastructure to address staffing shortages, manage increasing patient volumes, and meet growing demands for personalized care.
Regulatory approval processes continue streamlining to accommodate AI medical devices, encouraging innovation while maintaining safety standards. The FDA’s predetermined change control plans allow AI systems to improve continuously without requiring separate approvals for each update.
Healthcare organizations prioritize AI investments that demonstrate clear returns on investment through improved efficiency, reduced errors, and enhanced patient satisfaction. Administrative applications that automate routine tasks free healthcare professionals to focus on direct patient care.
Global expansion of AI healthcare applications addresses medical needs in underserved regions where traditional healthcare infrastructure remains limited. AI-powered diagnostic tools deployed through mobile devices extend specialist expertise to remote areas.
Innovation Opportunities
Precision medicine applications represent the most promising area for AI expansion, where genetic analysis combines with clinical data to create truly personalized treatment approaches. AI algorithms analyze individual genetic profiles, environmental factors, and lifestyle characteristics to predict disease risks.
Mental health applications of AI address growing demand for psychological services through intelligent chatbots, mood monitoring systems, and therapy recommendation engines. These tools provide continuous support for patients with depression, anxiety, and other mental health conditions.
Preventive care applications leverage AI to identify health risks before symptoms develop, enabling interventions that prevent disease progression. Wearable devices equipped with AI algorithms monitor vital signs, activity patterns, and biomarkers continuously.
Drug repurposing represents an efficient approach where AI identifies new therapeutic applications for existing medications. Machine learning algorithms analyze drug mechanisms, disease pathways, and patient outcomes to discover unexpected connections between approved drugs and untreated conditions. Healthcare organizations exploring these innovation opportunities often benefit from generative AI development services to create custom solutions tailored to their specific medical needs.
Industry Transformation Trends
Healthcare delivery models evolve toward integrated systems where AI coordinates care across multiple providers and settings. Electronic health records powered by AI automatically update patient information, schedule appointments, and coordinate treatment plans between primary care physicians, specialists, and ancillary services.
Telemedicine platforms enhanced with AI capabilities enable sophisticated remote consultations that rival in-person visits. AI algorithms analyze patient symptoms, vital signs, and medical history during virtual appointments, providing real-time decision support to healthcare providers.
Healthcare professionals’ roles shift toward collaborative partnerships with AI systems rather than competition or replacement. Physicians focus on complex decision-making, patient communication, and ethical considerations while AI handles routine data analysis, pattern recognition, and administrative tasks.
Medical specialization evolves as AI systems handle increasingly sophisticated diagnostic and treatment tasks. Radiologists transition from image interpretation to AI oversight and complex case management, while pathologists focus on integrating AI findings with clinical contexts to guide treatment decisions.
Frequently Asked Questions About AI in Healthcare
How does AI improve patient safety in hospitals?
AI improves patient safety through early warning systems that monitor vital signs, medication interactions, and fall risks continuously. These systems analyze patient data in real-time to predict sepsis, cardiac events, and other emergencies before they become life-threatening. AI also reduces medication errors by checking drug interactions and alerting healthcare providers to potential allergies or dangerous dosage combinations.
What types of medical imaging benefit most from AI analysis?
Chest X-rays, mammograms, CT scans, and MRI scans show the greatest improvement with AI analysis. AI systems excel at detecting pneumonia in chest X-rays, identifying breast cancer in mammograms, spotting blood clots in CT scans, and finding brain tumors in MRI images. These applications have received the most FDA approvals because they demonstrate clear accuracy improvements over traditional analysis methods.
Can AI systems work with existing electronic health record platforms?
Most modern AI systems integrate with major electronic health record platforms through standardized interfaces like HL7 FHIR. However, integration complexity varies depending on the specific EHR system and AI application. Healthcare organizations typically work with AI vendors to customize integration based on their existing technology infrastructure and workflow requirements.
What happens when AI diagnostic tools disagree with physician assessments?
Healthcare providers maintain final authority over all diagnostic decisions, regardless of AI recommendations. AI systems function as decision support tools that provide additional information for physician consideration. When disagreements occur, physicians can override AI suggestions based on their clinical judgment, patient interaction, and additional factors the AI system might not consider.
How long does it take to train healthcare staff on new AI systems?
Basic AI system training typically takes 1-3 days for most healthcare professionals, while specialized applications may require 1-2 weeks of training. Training duration depends on the complexity of the AI tool, the user’s technical background, and integration with existing workflows. Most AI vendors provide online training modules, hands-on workshops, and ongoing support to ensure successful adoption.
Do patients need to consent to AI analysis of their medical data?
Patient consent requirements for AI analysis vary by healthcare organization and specific application. Many healthcare systems include AI processing in their general consent forms for medical treatment. When AI systems process sensitive data or generate treatment recommendations, organizations may require specific informed consent that explains how AI tools will be used in the patient’s care.


